Global Tuberculosis Control PDF
Preview Global Tuberculosis Control
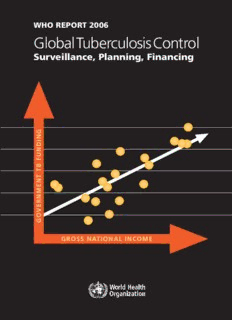
G WHO REPORT 2006 L O Global Tuberculosis Control B A Surveillance, Planning, Financing L T U B E The World Health Organization monitors R C the global tuberculosis epidemic and evaluates U L surveillance, planning and fi nancial data in support O of national TB control programmes. S I S G C N O I For further information about tuberculosis, D N N please contact: U T F Information Resource Centre HTM/STB R B World Health Organization O T 20 avenue Appia, CH-1211 Geneva 27, Switzerland L T fax +41 22 791 4285 N E [email protected] W M N H You can also visit our web site at: R O E www.who.int/tb V R O E G P O R GROSS NATIONAL INCOME T 2 0 0 6 ISBN 95 4 156314 1 ccoouuvv__AARRPP..iinndddd 11 1133..22..22000066 1177::3344::5544 WHO REPORT 2006 Global Tuberculosis Control Surveillance, Planning, Financing ii--vvii__AARRPP..iinndddd ii 1133..22..22000066 1188::4444::3377 WHO Library Cataloguing-in-Publication Data World Health Organization. Global tuberculosis control : surveillance, planning, fi nancing : WHO report 2006. 1.Tuberculosis, Pulmonary – prevention and control 2.Tuberculosis, Multidrug-resistant – drug therapy 4.Directly observed therapy 5.Treatment outcome 6.National health programmes – organization and adminisrtation 7.Financing, Health 7.Statistics I. Title. ISBN 92 4 156314 1 (NLM classifi cation: WF 300) WHO/HTM/TB/2006.362 Suggested citation: Global tuberculosis control: surveillance, planning, fi nancing. WHO report 2006. Geneva, World Health Organization (WHO/HTM/TB/2006.362). © WORLD HEALTH ORGANIZATION 2006 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to Marketing and Dissemination, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specifi c companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either express or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. For reasons of space, the names of Member States are sometimes shortened in certain fi gures. Cover: Gross national income per capita of 19 high-burden countries compared with the proportion of funds for TB control that is provided by their governments (rather than by donor agencies). Countries with a higher average income per capita tend to contribute more to the cost of TB control. The fi nancial contributions made by governments will be crucial to the success of The Global Plan to Stop TB, 2006–2015. The data are presented in detail in Figure 33 of the main text. Designed by minimum graphics Printed in Switzerland ii--vvii__AARRPP..iinndddd iiii 1133..22..22000066 1188::4444::3399 Contents Acknowledgements v Abbreviations vi Key points 1 Summary 2 Points clés 5 Résumé 6 Puntos clave 10 Resumen 11 Introduction 15 Methods Monitoring progress in TB control 17 Goals, target and indicators for TB control 17 Data collection and verifi cation 18 High-burden countries, WHO regions and other subregions of the world 18 DOTS classifi cation 18 DOTS coverage 19 Estimating TB incidence, prevalence and death rates 20 Case detection 21 Comparison of methods for evaluating case detection 22 Outcomes of treatment 22 DOTS implementation and planning 22 Collaborative TB/HIV activities 23 Surveillance and management of drug resistance 23 Financing TB control 24 Data collection 24 Data entry and analysis 25 GFATM contribution to TB control 26 Country reports compared with the Global Plan 26 Results Monitoring progress in TB control 27 Countries reporting to WHO 27 Case notifi cations and incidence estimates 27 DOTS coverage 30 Case detection 33 Comparison of methods for evaluating case detection 36 Outcomes of treatment 37 Trends in case detection and treatment success: overview of national DOTS programmes 41 Trends in prevalence and death rates 43 DOTS implementation and planning 43 Pursuing high-quality DOTS expansion and enhancement 43 Addressing TB/HIV, MDR-TB and other challenges 45 GLOBAL TUBERCULOSIS CONTROL | iii ii--vvii__AARRPP..iinndddd iiiiii 1133..22..22000066 1188::4444::3399 Engaging all care providers 49 Empowering people with TB, and communities 49 Financing TB control 50 Data received 50 Total NTP budgets and funding in high-burden countries 50 Total costs of TB control and funding in high-burden countries 52 Budgets and costs per patient 55 Expenditures in comparison with available funding and case detection 56 Budgets, funds and targets 57 GFATM contribution to TB control 59 NTP budgets by WHO region, HBCs and other countries 59 Costs: country reports compared with the Global Plan 59 Conclusions Monitoring progress in TB control 62 Case detection 62 Outcomes of treatment 62 Epidemiological trends and the impact of TB control 63 DOTS implementation and planning 64 DOTS expansion and the Stop TB Strategy 64 Laboratory diagnostic services 64 Human resource development 64 Collaborative TB/HIV activities 64 Management of drug resistance 65 TB, poverty and health systems 66 Advocacy, communication and social mobilization 66 Financing TB control 66 Annex 1 Profi les of high-burden countries 69 Annex 2 Regional and country data 137 Explanatory notes for regional and country data 139 Summary by WHO region 141 Africa 147 The Americas 163 Eastern Mediterranean 179 Europe 195 South-East Asia 211 Western Pacifi c 227 iv | WHO REPORT 2006 ii--vvii__AARRPP..iinndddd iivv 1133..22..22000066 1188::4444::3399 Acknowledgements The WHO Global TB Surveillance, Planning and Financing Project is coordinated by Christopher Dye, Léopold Blanc and Katherine Floyd. The 2006 report was written by Daniel Bleed, Christopher Dye, José Figueroa-Muñoz, Kather- ine Floyd, Mehran Hosseini, Eva Nathanson, Andrea Pantoja, Amy Piatek, Alasdair Reid, Catherine Watt, Brian Williams and Abigail Wright. The following WHO staff assisted in compiling, analysing and editing information: WHO HQ Geneva: Mohamed Aziz, Karin Bergström, Léopold Blanc, Karen Ciceri, Valérie Diaz, Giuliano Gargioni, Haileyesus Getahun, Andrea Godfrey, Malgorzata Grzemska, Ernesto Jaramillo, Jun-Wook Kwon, Knut Lönnroth, Rafael Lopez-Olarte, Dermot Maher, Pierre-Yves Norval, Paul Nunn, Salah-Eddine Ottmani, Thaddeus Pennas, Rose Pray, Mario Raviglione, Krystyna Ryszewska, Fabio Scano, Igor Toskin, Mukund Uplekar, Lana Velebit, Diana Weil, Matteo Zignol. WHO African Region: Ayodele Awe (Nigeria), Oumou Bah-Sow (AFRO), Joseph Imoko (Uganda), Joel Kangangi (Kenya), Bah Keita (AFRO, West Africa), Daniel Kibuga (AFRO), Motseng Makhetha (South Africa), Robert Makombe (AFRO), Giampaolo Mezzabotta (Uganda), Vainess Mfungwe (AFRO), Wilfred Nkhoma (AFRO), Angélica Salomão (Mozambique), Henriette Wembanyama (DR Congo). WHO Region of the Americas: Ademir Albuquerque (Brazil), Raimond Armengol (El Salvador), Marlene Francis (CAREC), Mirtha del Granado (AMRO), Juan Carlos Millan (Peru), Pilar Ramon-Pardo (AMRO), Rodolfo Rodriguez- Cruz (Brazil), Matías Villatoro (Brazil). WHO Eastern Mediterranean Region: Aaiyad Al Dulaymi Munim (Somalia), Samiha Baghdadi (EMRO), Yuriko Egami (Pakistan), Laura Gillini (Pakistan), Sevil Husseinova (Afghanistan), Akihiro Seita (EMRO), Ireneaus Sindani (Sudan). WHO European Region: Pierpaolo de Colombani (EURO), Irina Danilova (Russian Federation), Lucica Ditiu (Balkans), Wieslaw Jakubowiak (Russian Federation), Konstantin Malakhov (Russian Federation), Kestutis Miskinis (Ukraine), Andrey Mosneaga (Caucasus), Jerod Scholten (EURO), Gombogaram Tsogt (Central Asia), Elena Yurasova (EURO/Russian Federation), Richard Zaleskis (EURO). WHO South-East Asia Region: Marijke Becx-Bleumink (Bangladesh), Erwin Cooreman (SEARO), Christian Gunneberg (Nepal), Hans Kluge (Myanmar), Franky Loprang (Indonesia), Davide Manissero (Indonesia), Firdosi Mehta (Indonesia), Nani Nair (SEARO), Myo Paing (SEARO/Myanmar), Suvanand Sahu (India), Chawalit Tantinim- itkul (Thailand), Fraser Wares (India). WHO Western Pacifi c Region: Dong Il Ahn (WPRO), Maarten Bosman (Viet Nam), Daniel Chin (China), Philippe Glaziou (WPRO), Pratap Jayavanth (Cambodia), Wang Lixia (China), Pieter van Maaren (WPRO), Bernard Tomas (WPRO), Michael Voniatis (Philippines). The primary aim of this report is to share information from national TB control programmes. The data presented here are supplied largely by programme managers, who have been instrumental in driving much of the work on surveillance, planning and fi nancing. We thank all of them, and their staff, for their contributions. The WHO TB Surveillance, Planning and Financing Project is carried out with the fi nancial backing of USAID. The WHO DOTS Expansion Project is supported by funding from the governments of Australia, Belgium, Canada, Germany, Ireland, the Netherlands, Norway, Switzerland, the United Kingdom and the United States. Data for the European Region were collected and validated jointly with EuroTB, a dedicated European TB surveillance network funded by the European Commission; we thank Dennis Falzon of EuroTB for his collaboration. Rhehab Chimzizi and Tony Harries kindly allowed us to present their important data on antiretroviral therapy in Malawi. We also thank Pam Baillie, Kreena Govender and Sue Hobbs for their usual effi ciency in helping to get this report published by 24 March, World TB Day. Copies of Global tuberculosis control are available from the World Health Organization, 20 Avenue Appia, CH-1211 Geneva 27, Switzerland, and at www.who.int/tb. GLOBAL TUBERCULOSIS CONTROL | v ii--vvii__AARRPP..iinndddd vv 1133..22..22000066 1188::4444::4400 Abbreviations ACSM Advocacy, communication and social IPT Isoniazid preventive therapy mobilization ISAC Intensifi ed support and action in countries, AFB Acid-fast bacilli an emergency initiative to reach targets for AFR WHO African Region DOTS implementation by 2005 AFRO WHO Regional Offi ce for Africa IUATLD International Union Against Tuberculosis and AIDS Acquired immunodefi ciency syndrome Lung Disease AMR WHO Region of the Americas JICA Japan International Cooperation Agency AMRO WHO Regional Offi ce for the Americas LACEN Brazilian public health laboratories ART Antiretroviral therapy LGU Local government unit BPHS Basic package of health-care services LGA Local government area BRAC Bangladesh Rural Advancement Committee MDG Millennium Development Goal CAREC Caribbean Epidemiology Centre MDR Multidrug resistance CDP Community DOT providers MDR-TB Multidrug-resistant tuberculosis CPT Co-trimoxazole preventive therapy MoH Ministry of Health DCT Diagnostic counselling and testing for HIV MoPH Ministry of Public Health DFB Damien Foundation Belgium MSH Management Sciences for Health DFID UK Department for International NAP National AIDS control programme or Development equivalent DoH Department of Health NGO Nongovernmental organization DOT Directly observed treatment NHLS National Health Laboratory Services DOTS The internationally recommended strategy NPO National professional offi cer (WHO- for TB control appointed) DRS Drug resistance surveillance or survey NRL National reference laboratory DST Drug susceptibility testing NTP National tuberculosis control programme or EMR WHO Eastern Mediterranean Region equivalent EMRO WHO Regional Offi ce for the Eastern PAHO Pan-American Health Organization Mediterranean PAL Practical Approach to Lung Health EQA External quality assurance PhilTIPS Philippine Tuberculosis Initiatives for the EUR WHO European Region Private Sector EURO WHO Regional Offi ce for Europe PPM Public–private or public–public mix FDC Fixed-dose combination (or FDC anti-TB SEAR WHO South-East Asia Region drug) SEARO WHO Regional Offi ce for South-East Asia FIDELIS Fund for Innovative DOTS Expansion, SILTB Brazilian laboratory information system managed by IUATLD SINAN Brazilian health information system GDF Global TB Drug Facility TB Tuberculosis GFATM Global Fund to Fight AIDS, Tuberculosis and TBCTA Tuberculosis Coalition for Technical Malaria Assistance GLC Green Light Committee UNAIDS Joint United Nations Programme on HIV/ GLRA German Leprosy and TB Relief Association AIDS GNI Gross national income UNDP United Nations Development Programme HBC High-burden country of which there are 22 USAID United States Agency for International that account for approximately 80% of all Development new TB cases arising each year VCT Voluntary counselling and testing for HIV HEW Health extension workers infection HIV Human immunodefi ciency virus VHV Village health volunteers HNPSP Health Nutrition and Population Sector WHO World Health Organization Programme WPR WHO Western Pacifi c Region HR Human resource(s) WPRO WHO Regional Offi ce for the Western IEC Information, education, communication Pacifi c vi | WHO REPORT 2006 ii--vvii__AARRPP..iinndddd vvii 1133..22..22000066 1188::4444::4400 Key points TB EPIDEMIC • There were 9 million new TB cases and approximately 2 million TB deaths in 2004. • The number of TB cases was stable or falling in 5 of 6 WHO regions, but growing in Africa where the TB epidemic is still driven by the spread of HIV. • More than 80% of all TB patients live in sub-Saharan Africa and Asia. DOTS AND THE NEW STOP TB STRATEGY • DOTS, which remains at the heart of the new Stop TB Strategy, was being applied in 183 countries in 2004; population coverage was complete in 9 of 22 high-burden countries (HBCs), and almost complete in 5 others. • Expanding areas of work within the new strategy include: community and NGO participation in TB care; advocacy, communication and social mobilization; and improved management of multidrug-resistant TB and TB/HIV. • Six Asian countries and Kenya have already improved links between national TB control programmes (NTPs), hospitals and other health-care providers, but PPM-DOTS is still at an early stage in most other HBCs. • Areas of particular weakness are laboratory services, human resource development and the monitoring of TB/HIV control. FINANCES • The total cost of TB control in 2006, including NTP budgets and costs to the general health-care system, has grown to US$ 1.6 billion in the 22 HBCs. This increases to US$ 2.0 billion for all 74 countries that provided fi nancial data. • Funding to support TB control in the 22 HBCs has increased by almost US$ 500 million since 2002, reaching US$ 1.4 billion in 2006. • Governments of the wealthier HBCs (notably Brazil, China, the Russian Federation and South Africa) provide most of the funding needed for TB control in their countries; other countries rely more on grants from donors, including the Global Fund to Fight AIDS, Tuberculosis and Malaria. • The funding gap reported by the 22 HBCs for 2006 was US$ 141 million; it was US$ 180 million in total for the 74 countries that reported data. • NTP budgets for 2006 are broadly in line with the Global Plan to Stop TB, 2006–2015, except for TB/HIV control where NTP budgets are much lower. TARGETS • Case detection was 53% globally in 2004, and is likely to exceed 60% in 2005, falling short of the 70% target. • Treatment success was 82% in the 2003 cohort of 1.7 million patients, approaching the 85% target. • Three WHO regions are expected to have met both of the 2005 targets: the Region of the Americas and the South-East Asia and Western Pacifi c regions. • At least 7 HBCs should have met the 2005 targets: Cambodia, China, India, Indonesia, Myanmar, the Philippines and Viet Nam. • Implementation of the Global Plan is expected to reverse the rise in incidence globally by 2015, as specifi ed by the Millennium Development Goals, and to halve 1990 prevalence and death rates globally and in most regions by 2015, though not in Africa and eastern Europe. GLOBAL TUBERCULOSIS CONTROL | 1 0011--6688__AARRPP..iinndddd 11 2222..22..22000066 77::4433::4466 Summary Background and methods 7. The 2.1 million smear-positive cases notifi ed by DOTS programmes in 2004 represent 53% of the estimated inci- 1. The 10th WHO annual report on surveillance, planning dence. The increment in smear-positive cases notifi ed un- and fi nancing for global tuberculosis (TB) control includes der DOTS between 2003 and 2004 (350 000) was greater data on case notifi cations, treatment outcomes, activities, than ever before (the average annual increment from budgets, costs and expenditures. Results are given for all 1995–2000 was 134 000). If the observed acceleration in national TB control programmes (NTPs) that have reported case-fi nding is maintained, DOTS programmes will detect to WHO, although the emphasis is on progress in 22 high- more than 60% of cases in 2005, but they will fall short of burden countries (HBCs). the 70% target. 2. Eleven consecutive years of data (1994–2004) are now 8. The acceleration in case-fi nding since 2000 has been available to assess progress towards the Millennium Devel- observed in the case reports from all sources, as well as opment Goals (MDGs) for TB control, and towards targets from DOTS programmes. We infer that case detection has set by the World Health Assembly (WHA) and the Stop TB continued to improve because patients are being reported Partnership. WHA targets are to detect, by 2005, 70% of from new sources, including public and private clinics and new sputum smear-positive cases and to successfully treat hospitals, especially in the South-East Asia and Western 85% of these cases. MDG target 8 (of 18) is to have halted Pacifi c regions. and begun to reverse the TB incidence rate by 2015. The Stop TB Partnership has endorsed additional targets of 9. Of the additional smear-positive cases reported under halving 1990 prevalence and deaths rates by 2015. DOTS in 2004, three-quarters (75%) were in China, India and Indonesia. These three countries have been driving the Improving case detection and treatment global acceleration in case detection, backed by Bangla- 3. A total of 200 (of 211) countries and territories report- desh, Brazil and Myanmar. Among patients who suffered a ed to WHO on their strategies for TB control, and on TB fi rst episode of TB in 2004 but were not detected by DOTS case notifi cations and/or treatment outcomes. programmes, 61% lived in eight countries: Bangladesh, China, Ethiopia, India, Indonesia, Nigeria, Pakistan and the 4. Using surveillance and survey data to update estimates Russian Federation. of incidence, we calculate that there were 8.9 million new cases of TB in 2004 (140/100 000 population), of which 10. The smear-positive case detection rate within estab- 3.9 million (62/100 000) were smear-positive and 741 000 lished DOTS areas remained stable at an average of 51% up were in adults infected with the human immunodefi ciency to 2001, but increased to 64% in 2004. These recent im- virus (HIV). There were 14.6 million prevalent cases (229/ provements in case-fi nding within DOTS areas have taken 100 000), of which 6.1 million were smear-positive (95/ place predominantly in Bangladesh, Brazil, China, India, In- 100 000). More than 80% of all new TB patients in 2004 donesia, Myanmar and the Philippines. were in the African, South-East Asia and Western Pacifi c 11. While WHO measures case detection principally with regions. An estimated 1.7 million people (27/100 000) died reference to smear-positive disease, statistics for detection from TB in 2004, including those coinfected with HIV based on other diagnostic methods give a different view of (248 000). programme performance. A comparison of 25 European 5. A total of 183 countries and territories were implement- countries in 2004 showed that the proportion of estimated ing the DOTS strategy during 2004. By the end of 2004, smear-positive cases detected was always higher than the 83% of the world’s population lived in countries, or parts of proportion of estimated culture-positive cases detected, but countries, covered by DOTS. DOTS programmes notifi ed 4.4 lower than the proportion of all estimated TB cases detected. million new and relapse TB cases in 2004, of which 2.1 mil- In the Region of the Americas, by contrast, smear-positive lion were new smear-positive. In total, 21.5 million TB pa- detection rates were typically higher than the detection rates tients, and 10.7 million smear-positive patients, were treated of all TB cases. These differences need further investigation in DOTS programmes over the 10 years 1995–2004. because they are likely to be important in evaluating TB epi- demiology and control now, and when assessing the role of 6. At the end of 2004, DOTS expansion was complete in new and more sensitive diagnostic tools. nine HBCs and nearing completion in fi ve others. Pakistan reported full DOTS coverage by the end of 2005, and cov- 12. Treatment success in the 2003 DOTS cohort of 1.7 mil- erage has increased considerably in Afghanistan, Brazil, In- lion patients was 82% on average, edging closer to the dia and the Russian Federation. 85% target. As in previous DOTS cohorts, treatment suc- 2 | WHO REPORT 2006 0011--6688__AARRPP..iinndddd 22 2222..22..22000066 77::4433::4488 cess was substantially below average in the African Region special attention include national reference laboratories, (72%) and the European Region (75%). The relatively poor external quality assurance for all laboratories, and the de- outcomes in these two regions can be attributed, in part, velopment of capacity and infrastructure for culture and for to the complications of HIV coinfection and drug resist- drug susceptibility testing. ance, respectively. Equally important, though, is the failure 18. A total of 15 HBCs have plans for the development of of DOTS programmes in these two regions to monitor the human resources, but most of these plans are limited to outcome of treatment for all patients. To reach the target training; 18 HBCs listed investments in staff among the fi ve of 85% treatment success globally, a special effort must be most benefi cial ways to improve DOTS and to strengthen made to improve cure rates in the African and European health systems. NTPs supported health system development regions. during 2005 mostly by bringing TB control programmes into 13. Based on case reports and WHO estimates, 26 coun- line with the process of health service decentralization. tries had reached the targets for case detection and treat- 19. The decentralization of diagnostic and treatment serv- ment success by the end of 2004. The Philippines and Viet ices is intended to improve access for all patients, but espe- Nam were the only HBCs among them. Cambodia, China, cially for those who are poor. NTPs are beginning to involve India, Indonesia and Myanmar may also have reached the communities and NGOs so as to improve awareness of, and targets by the end of 2005 (i.e. a total of 7 out of 22 HBCs), access to, these services. but this will not be known until the end of 2006. 20. Community participation in TB control is part of NTP Epidemiological trends and the impact of strategy in 14 HBCs. The number of HBCs with national TB control strategies for advocacy, communication and social mobili- zation (ACSM) has increased from 2 in 2002 to 11 in 2005, 14. In 2004, per capita TB incidence was stable or falling in and is expected to reach 19 by 2007. fi ve out of six WHO regions, but growing at 0.6% per year globally. The exception is the African Region, where TB in- 21. HBCs are in various stages of developing collaborations cidence was still rising, following the spread of HIV. How- within and among public and private health sectors ever, the annual increase in case notifi cations from the (through PPM-DOTS). While Bangladesh, China, India, In- African Region is declining each year, probably because the donesia, Kenya, Myanmar and the Philippines have already HIV epidemics in African countries are also slowing. In east- improved links between NTPs, hospitals and other health- ern Europe (mostly countries of the former Soviet Union), care providers, PPM-DOTS is still at an early stage in most incidence per capita increased during the 1990s, but other HBCs. peaked around 2001, and has since fallen. 22. The treatment of drug-resistant TB is still inadequate in 15. There are few good data with which to establish TB many countries. In some, laboratory diagnosis is of poor prevalence and death rates for the MDG baseline year of quality; others lack national policies on MDR-TB manage- 1990 and for 2004. Our best estimates are that prevalence ment; fi rst- and second-line anti-TB drugs of uncertain fell from 297 per 100 000 population globally in 1990 to quality are widely available; and large numbers of MDR-TB 229 per 100 000 in 2004 (including HIV-positive TB pa- patients are subject, outside NTPs, to inappropriate diag- tients), partly as a consequence of DOTS expansion. TB nostic and treatment procedures. Part of the remedy will be mortality declined from 29 per 100 000 in 1990 to 27 per to implement widely new WHO guidelines on the pro- 100 000 in 2004. But for the strongly adverse trends in grammatic management of drug-resistant TB. Africa, prevalence and death rates would be falling more 23. Many of the countries that are most affected by HIV/ quickly worldwide. AIDS have national plans and policies for collaborative TB/ 16. The epidemiological forecast for 2005 and beyond is HIV activities, and for providing ART. But most have still to set out in the Global Plan to Stop TB, 2006–2015, which make ART available to more than a small proportion of eli- will cost US$ 56 billion to implement. The improvements in gible people. In those countries that have rapidly increased case detection proposed in the Global Plan, when imple- access to ART, and where the prevalence of HIV infection is mented alongside other elements of the Stop TB Strategy, high, the challenge will be to maintain access to and fund should reverse the rise in TB incidence by 2015, and halve ART without draining resources from other programmes. prevalence and death rates globally and in all regions ex- cept Africa and eastern Europe. Financing DOTS expansion 24. Financial reports were received from 140 out of 211 DOTS implementation and planning (66%) countries. These countries account for 91% of the 17. Although laboratory networks have expanded through estimated global burden of TB. Complete budget data for national and international efforts, TB laboratory services 2005 and 2006 were reported by 87 and 71 countries re- need to be improved in many countries. The areas requiring spectively, while 73 countries provided complete expendi- GLOBAL TUBERCULOSIS CONTROL | 3 0011--6688__AARRPP..iinndddd 33 2222..22..22000066 77::4433::4488
Description: